In this blog, Karen Morley, who in 2018 wrote here about her experiences of OCD (obsessive compulsive disorder) and how evidence helped her, tells us what has happened since, including the impact of the COVID-19 pandemic on her mental health, the challenges, and things she has found empowering.
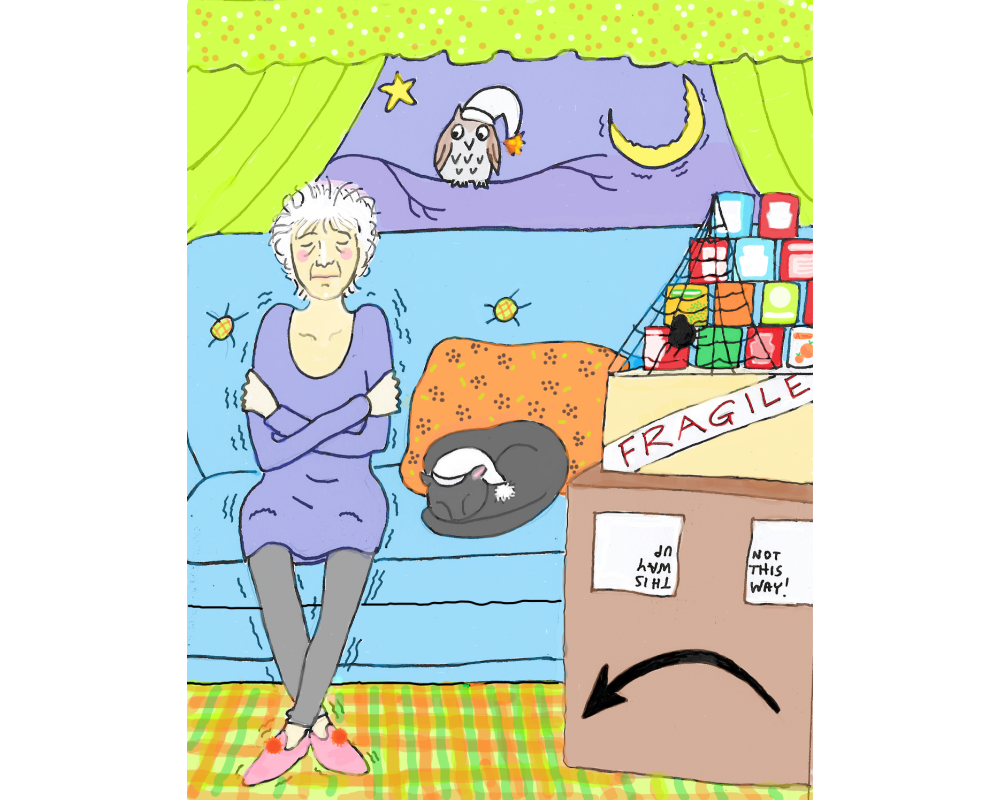
Featured image: ‘Shaking’ by Karen Morley. “This represents the situation I describe in the section ‘And then came Covid’: I quarantined my food for anything up to 28 days. I sat on my sofa and shook like a leaf, trying to calm my fight/flight response. I left my curtains and doors open so I didn’t have to touch them; my hallway was full of boxes waiting to be opened.’ I’m pleased to be able to look back on this with some amusement now. At the time, it really wasn’t funny.”
Take-home points
Since I wrote about it in 2018, in the blog My OCD story: evidence-based medicine to the rescue!, I’ve been getting to know my disorder, contamination OCD. I know stress triggers it and that caring for my mum, who had dementia, brought on a difficult episode. After she died in 2017 I continued with my medication until I was invited by my GP to take part in the ANTLER Randomised Controlled Trial, Antidepressant medication to prevent depression relapse in primary care, which looked at discontinuation after longer-term use. After a year of taking pills for the trialClinical trials are research studies involving people who use healthcare services. They often compare a new or different treatment with the best treatment currently available. This is to test whether the new or different treatment is safe, effective and any better than what is currently used. No matter how promising a new treatment may appear during tests in a laboratory, it must go through clinical trials before its benefits and risks can really be known. that were then revealed to be placeboAn intervention that appears to be the same as that which is being assessed but does not have the active component. For example, a placebo could be a tablet made of sugar, compared with a tablet containing a medicine. pills, I decided not to restart my medication. But as winter approached and my symptoms worsened, I got myself back on the IAPT (Improving Access to Psychological Therapies programme) waiting list.
And then came Covid
The World Health Organization, in March 2022, reported that the pandemic had caused a 25% global increase in anxiety and depression. Those with pre-existing mental health conditions were among those who were hit the hardest. I was one of many who relapsed.
I think it was a combination of things: the isolation, the barrage of news and social media reports, the frightening images in the public information campaign, the emphasis on hand-washing, what seemed to me to be the dreadfully inadequate government response, the uncertainty and shock, and, above all, the overwhelming suffering of people everywhere.
I’d been telling myself that touching things I was afraid of was okay. Now, suddenly, it seemed it wasn’t. I searched repeatedly for information about the duration of contamination on surfaces. My obsession was particularly focussed on food packaging – remember when we quarantined our shopping? Well, to begin with I quarantined mine for the maximum time that contamination was said to persist in a laboratory: anything up to 28 days. I lived on frozen, canned and long-life food, supplemented with vitamin tablets.
I was exceedingly anxious. I sat on my sofa and shook like a leaf, trying to calm my fight/flight response. I left my curtains and doors open so I didn’t have to touch them; my hallway was full of boxes waiting to be opened and I used so much electricity on washing damp towels and discarded clothing that you can track my progress through the graph of my energy consumption. I lost lots of weight.
Seeking help
Waiting
Of course, I got in touch with my GP and resumed my medication but the wait for it to take effect seemed endless.
I called IAPT to say my symptoms were worse and I wasn’t eating properly. I was told, sympathetically, that the waiting list was extremely long because both demand and treatmentSomething done with the aim of improving health or relieving suffering. For example, medicines, surgery, psychological and physical therapies, diet and exercise changes. availability had been affected by the pandemic. I was sent some links to online self-help sites for general and pandemic-related anxiety, given contacts in case of a crisis and sent away to do some more waiting. They’d let me know when I reached 40th on the list.
I hung on…
There are people whose illness is far worse than mine. I don’t know how they bear it. The symptoms of my mental health disorder at their worst were as all-pervading and difficult to endure as physical pain – but there is no parity in treatment and support. I felt wretched, debilitated and confined to my home by overwhelming fear without the intolerable inequities faced by so many others – and which in themselves predisposed people to poorer mental health during the pandemic as well as to worse physical health across the globe.
Personalised treatment
I paid privately for a counsellor my GP recommended. I can afford to pay but it’s quite beyond so many people’s means. Why should anyone be deprived of support? It’s monstrous.
The counsellor was wonderful: sensitive, well-informed, and a forensic listener. I felt the sessions were completely personalised and that we worked in partnership. At my request, we started some Exposure and Response Prevention but the counselling went beyond this. She helped me understand my mental well-being in useful, effective ways.
By the time my IAPT CBT treatment became available, about fifteen months after I first applied, I was already better able to manage my symptoms. My CBT was an entirely different experience this time. No longer a carer, I felt less pressured and better able to engage. But I also had an excellent and well-trained tele-therapist who tailored the sessions to suit me and gave me a good understanding of the way the approaches we took were meant to work.
A toolkit of strategies
I now have a toolkit full of strategies to help me with what I have come to accept will be a lifetime of managing my conditions. Two of the key ones for me have been mindfulness and self compassion. Mindfulness meditation with its focus in the present moment makes me feel more grounded. It helps if I accept my OCD anxiety rather than fighting it. I see it as something intended to be helpful that has gone wrong, rather than a bully I need to stand up to. It also helps if I show myself understanding rather than beating myself up.
These approaches seem to lower my resistance to taking action. For those times when anxiety seemed overwhelming, breathing exercises with progressive relaxation were helpful. I appreciate that what works for me won’t work for everyone, which is why the personalisation of treatment is so important.
Taking part in research has been empowering
As well as taking part in the ANTLER trial, I was an author on a Cochrane Review about OCD in people with autism spectrum disorder. This has given me several things:
My perspective has changed. Preparing for additional, as yet unpublished research, I’ve taken part in meetings with fellow experiencers of OCD. I can see that my own OCD behaviours, odd as they seem, aren’t personal quirks or weaknesses but symptoms, shared by many others, and this is comforting and empowering.
I’ve learned more about my condition from preparatory reading, screening abstracts, the insights of the author team and people with OCD. It’s interesting in itself to learn about the interplay of biology, disposition and experience, making connections with one’s own case. It tells me that knowledge of the condition is evolving, and no one thoroughly understands it, which encourages me to ask questions of health professionals.
I’ve learned about the lack of evidence about this condition and the persistent need for investment and consumer‘Consumer’ is Cochrane’s preferred term for patients (or someone with personal experience of a health condition), care-givers or family members of someone with a health condition. (https://consumers.cochrane.org)* involvement in research. For instance, I haven’t been able to find any evidence of OCD research prioritisation that involves consumers. Perhaps readers know otherwise but I should like to see that addressed soon. I’ve also felt good about contributing to research that will help address the evidence gaps.
New/enhanced skills. I have a variety of new and developing skills, from getting to know review software and practising screening to accepting what I don’t know without shame and actually daring to make suggestions. I see the importance of giving time and validation to others’ human and emotional experience of OCD and I better appreciate the value of qualitative research as one way of exploring this; I also wonder if there are better ways to align consumers’ needs and experience with research.
I’m now a more confident partner in making shared decisions about my health
I have a new GP who is supportive and seems very open to shared decision-making, but I think I’ve also become more confident. I put this down to the gains I have made through research participation, longer experience of the disorder, and overcoming my own sense of stigma – partly because during the isolation of the pandemic I’ve come to care less about how I’m perceived by others. My counsellor has shown me my right to preserve my own boundaries. I prepare as much as I can before an appointment, finding my information from trustworthy sources, then I say what it is that I want and ask for information more directly.
Now I am trying to wean myself off my medication, the Selective Serotonin Reuptake Inhibitor, fluoxetine. Evidence that might help me in shared decision-making seems scarce, as is trenchantly expressed in expert and consumer Dr Mark Horowitz’s brilliant blog for Evidently Cochrane, “Stopping antidepressants: what is the best way to come off them?“, which refers to the Cochrane Review Approaches for discontinuation versus continuation of long‐term antidepressant use for depressive and anxiety disorders in adults (April 2021), led by Ellen Van Leeuwen, of which he was an author.
The authors concluded, ‘We cannot make any firm conclusions about effects and safetyRefers to serious adverse effects, such as those that threaten life, require or prolong hospitalization, result in permanent disability, or cause birth defects. of the approaches studied to date.’ However, I asked my GP if I could taper slowly, which seems to be the emerging view, as can be seen in the guidance from the Royal College of Psychiatrists: Stopping antidepressants, which Dr Horowitz points out was strongly influenced by people with lived experience.
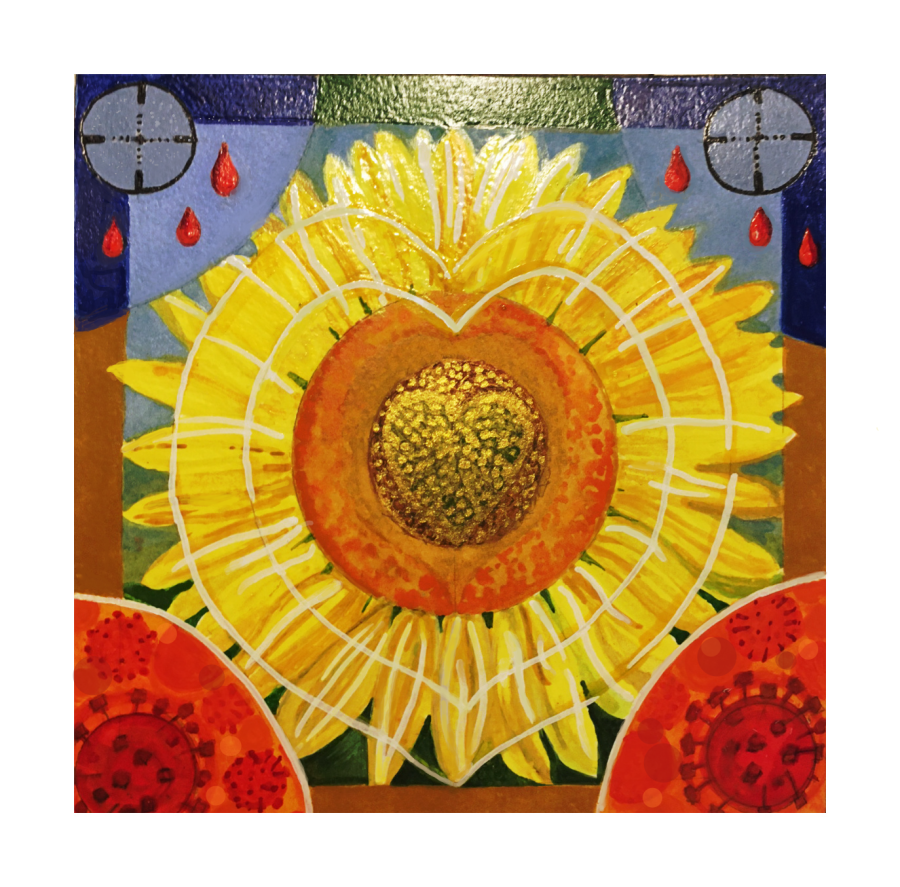
I find drawing and painting are helpful ways to cope with anxiety. In this mixed media illustration, I tried to represent the power of practical compassion in a threatening world. The sunflower is Ukraine’s national flower; the blue and gold of its flag represent fields of grain under a blue sky. I wanted to show radiance pushing back the shadows of the coronavirus and of violence, symbolised by the gunsights and the rain of blood, or fire. I had in my mind the quotation I used in my conclusion: ‘We must love one another or die’.
We are living in times of anxiety and trauma that affect the mental health of millions
Right now, the plight of the people of Ukraine is adding to the horrific sum of unrelenting war trauma around the world; the Covid pandemic has brought bereavement and suffering on a staggering scale; and poverty increasingly injures the most vulnerable. Alongside all this, my personal experience of OCD pales into insignificance. I am one of the lucky ones. Surely our current global emergencies show us humanity’s interconnectedness? What hurts one, hurts us all. Callous ideologies, greed, inequity and unthinkable disregard for people’s lives cause, exacerbate and prolong illness. They are raising a tsunami of mental disorders. We need to demonstrate compassion, not just through sympathy and worthy aspiration, but through timely practical measures that will benefit all of us. We need to fight for them.
W H Auden didn’t like his poem, September 1, 1939, or the line we all remember: ‘We must love one another or die.’ It seems to me to be the starkest of truths.
If you’d like to get involved in research:
NIHR Be Part of Research – you can search by topic and location.
*‘Consumer’ is the term used by Cochrane to denote a wide range of people, including patients (or people with personal experience of a healthcare condition), health and social care service users, caregivers and family members and people who represent or are advocates for patients and carers.
Karen Morley has nothing to disclose.


Hi,
I have read your article and found it very interesting. Thanks for the write-up.
Karen, thank you for your brave detailing of the recent journey you’ve been experiencing-putting this in the public domain is very generous. Offering others, with lived experience, opportunities to get involved with Cochrane, is likely to be beneficially life-changing.
Wow, Karen! Thank you for sharing your story and inspiring others to get involved in research!